My Grown-Up Christmas List (2020)
Back by popular demand… My Grown Up Christmas List! And just in time for Giving Tuesday. We may all have a Grown Up 2020 Christmas List this year with wishes like a COVID cure, an end to social distancing, and political peace!
This 1992 classic Christmas song (can I call it that?!) by Amy Grant is one of my favorites, as it takes my memory back to a time when I was beginning life as a “grown up” yet in retrospect, a time that was so simple and sweet! She sings about having outgrown the simplistic Christmas wishes of childhood and dreaming now of the intangible “gifts” that bring about a better world… peace on earth, an end to loneliness, healing of the human soul, unending love… Looking beyond ourselves and to a world in need. Isn’t this the very essence of Christmas? That God in His deep love for us found a way to rescue our human souls and bring LIGHT to a dark world… And now we, as His ambassadors, are to be that LIGHT to others, sharing the promise of His hope and love.
In sitting down to write about our grown-up wishes this year, it jumped out ironically to me that this song is from the album entitled “Home for Christmas”… We have moved from Kenya back to the USA, and “home” is currently a confusing and debated topic in our little family. As we seek to form new traditions and engage in our new community, our hearts are still tightly bound to our Kenyan community, and to the needs in which we have invested deeply over the past seven years.
If you have followed our family’s story at all, then you know that training surgeons for Africa is the “WHY” of why we moved to Kenya in 2014. So many African communities do not have access to basic surgical care, which brings a heavy burden of disease and death. At Tenwek through the PAACS training program, we had the privilege of training young doctors who are followers of Jesus and desire to use their gifts and abilities to serve the needs of their local communities and train others. It is a true multiplying ministry! Almost all of the surgeons who graduated during our six years there are working in mission hospitals and/or training other surgeons and young doctors. Three of our graduates (Drs. Blasto, Mbithi, and Kanyi) even joined together and started their own faith-based residency program at another mission hospital. And Heath turned over the Tenwek program leadership to one of our graduates, Dr. Liz Mwachiro. Although the Lord led our path back to the USA for now, we see this change in location as an evolution of our ministry, not a cessation. The “WHY” that led us to Africa still exists. We have faith that the Lord will work through our Kenyan colleagues to continue this vision. And we will stay involved in ways that empower and support them in their work.
One of the best ways we can help support this ministry is to continue to raise awareness of the need and finances to keep it going. It is expensive to train doctors. This faith-based training program depends completely on donations. So many of you have invested with us in this vision over the past several years!
Will you consider giving again this year toward this multiplying mission of training young doctors in Kenya to bring the love and hope of Jesus to their communities through compassionate and high-quality healthcare?
This is an investment like no other, a gift that truly keeps on giving for many years to come with both direct and eternal rewards!
Give to the Surgery Residency Fund to support the ongoing cost of training young surgeons at Tenwek. Two new residents, Ian Simel and Oscar Rotich, will join the eight other general surgery trainees in January.
Or give to the OB/GYN Residency Fund to support the NEW program expected to start in July. We are so excited to see this vision of ministry put in place to train OB/GYN specialists. Maternal and newborn care is a greatly neglected field in much of Africa, and this will be the first training program of its kind!
We remain volunteers with WGM and will keep a ministry account as well, which we will be using to help support needs that arise in the OB/GYN and Surgery residency programs throughout the year.
Click on any of these three links above to go directly to that online giving page. 100% of your donations will go to support these projects.




This Christmas season, I pray that God’s LIGHT will AWAKEN our souls to His work all around us, SHINE into the darkest corners or our hearts and minds, and POUR out to others.
THANK YOU for investing prayers, time, and funding into our ministry at Tenwek Hospital over the years, and THANK YOU for considering ongoing support of these endeavors.
Your steadfast love, O LORD, extends to the heavens, your faithfulness to the clouds…For with you is the fountain of life; in your LIGHT do we see light. ~Psalm 36: 5,9
Again Jesus spoke to them saying, “I am the light of the world. Whoever follows me will not walk in darkness, but will have the light of life.” ~John 8:12
Favorite Pics of 2019
“But Mary treasured up all these things and pondered them in her heart.” ~Luke 2:19
At the end of each year, I often find myself wishing that I had blogged, communicated, and documented more. Those are not the things that I usually prioritize in the midst of daily life. And in this era of technology and social media there is always temptation to feel as if that which isn’t documented doesn’t “count” for much. But this advent season, the above verse stood out to me in new ways. I’ve treasured up and pondered so many things in my heart this year… things that were good, hard, messy, heart-wrenching, inspiring, miraculous, beautiful. What have you treasured up and pondered?
Here are a few of my favorite pics from 2019, and here’s to more pondering in 2020!














My Grown Up Christmas List (2019)
Well folks, here it is…My Grown Up Christmas List for 2019! This year, our biggest wish is focused on those individuals with whom we spend our everyday lives… the Tenwek surgical residents. Could you help train a surgeon for East Africa? If that’s not the ultimate “gift that keeps on giving,” then I don’t know what is!
If you have followed our family’s story at all, then you know that training surgeons for Africa is the “WHY” of why we moved to Kenya in 2014. The need is shocking. So many African people do not have access to basic surgical care. Global health experts are increasingly realizing the great burden of disability and death that this lack brings to a community. Many places in Africa have only one surgeon to serve a population of 250,000. In other even lower resourced areas, there may be only one surgeon for up to 2.5 million people. To put this in perspective, the WHO recommends a minimum of one surgeon for 20,000 people. Our home area, Knox County TN, probably has about 40 general surgeons for 450,000. Imagine if we had only two surgeons in our whole county… that’s the situation in much of Africa (or worse!).
At Tenwek Hospital, we have the additional benefit of being able to mentor and disciple our surgical residents toward spiritual maturity and leadership abilities so that they can address the needs of the whole person and minister to their patients spiritually, offering hope and healing through Jesus to those who are suffering. These young doctors are committed to staying in Africa to help meet the needs of their communities. We see this happening, and we are so excited to see what the future brings with them leading the way.

Heath with last year’s surgical graduates
But…it is expensive to train doctors. It costs about 20K USD per resident per year for training costs. This compares to 120-145K USD per resident per year in the U.S. This provides a living stipend, educational supplies, support staff, exam fees, conference costs, and more. The costs for our program are completely supported by donors, and we need more partners to help support these residents into 2020. Would you consider supporting a surgical trainee? One hundred percent of your donations here go toward our residency training costs.
Meet our new first year residents to begin in January…

We have known Mercy since 2015 when she rotated at Tenwek Hospital as a medical student. She returned to Tenwek for internship, then was hired by the OB/GYN department where she has worked for the past 1.5 years. She has proven herself to be highly competent and caring. Mercy sees surgery as an effective way to use her abilities to share Christ with others and wants to serve in a needy area of Kenya.

Violet also came to Tenwek as a medical student in 2015, returned for internship, and then was hired by the cardiothoracic surgery department where she has worked for 1.5 years. Violet has also been in our mentor group for the past year. She is tenacious and bright, with a tender heart for her patients. Violet has a special passion for cardiac patients and hopes to eventually pursue training in that specialty area.

Yves is from Burundi, where the surgical need is among the highest in this region of the world. Yves came to Tenwek in January 2018 was hired as a general practitioner on the cardiothoracic surgery service with hopes of joining surgery residency. Compelled by the great need in his home country, Yves hopes to return to Burundi after residency as a fully trained surgeon to serve his community.
These three doctors will begin the five-year residency program at Tenwek in January. We are so excited for them and have such hope and confidence in how God will use them. Help us train these bright and motivated young surgeons to meet the needs of Sub-saharan Africa. Your gifts really make a difference here!
There are 2 ways to give. You can give directly to the Tenwek Surgical Residency Fund by clicking here. Alternatively you can give to our family’s ministry fund and we will direct all funds raised during this Christmas season to the surgical training program.

Unexpected Outcomes
It seems that episodes of profound discouragement are a regular part of the missionary surgeon’s diet. Day after day we toil alongside incredibly sick patients to bring healing, and too many times the outcomes are poor. Whether from patients arriving late in a disease course, or from underlying nutritional deficits, the outcome is often grim. Often these patients are children and their untimely death carries added sting. Other times, in our resource limited setting, resources are…well…limited. This past week I helped care for a patient injured in a car crash who required surgery for a bleeding spleen and liver. The team that operated on him did the right things and stopped the bleeding. However, after receiving 2 units of blood the blood bank was depleted. Hours after his operation he received additional units of blood, but the many hours of low blood pressure had taken their toll on the patient’s kidneys, lungs, and liver. A few days later he died from multi-organ failure.
Nevertheless, there are successes and at times these moments will catch me off guard by challenging my chronic discouragement and fatigued compassion. Recently, the critical care nurses at Tenwek put on a “Critical Care Day” to celebrate and draw attention to the some of the gains that have been made in providing care to the sickest of sick at our hospital. I arrived that morning tired from a couple of busy weeks of work. I was scheduled to give a lecture on how to care for the critically-ill trauma patient and anxious to get this done so that I could focus on wrapping up the work week. As the day unfolded, however, I was blown away by what the nurses had put together. Once again, Kenyan ideals of community and thanksgiving collided with my American ideals of efficiency and productivity. Thankfully, the result for me was unexpected joy in seeing God’s hand at work.
The day started in typical Kenyan fashion with speeches from numerous stake holders including a surprise speech from me (at least I was surprised). Hymns followed speeches, and a sermon followed the hymns. By mid-morning I was checking my watch so frequently that I began to wonder if my watch was broken and stuck on the same time. Following a obligatory chai break, which was now an hour overdue, the conference resumed. Time to get down to business. But before the educational part of the day could start, some additional introductions were made. Two patients who had survived major illnesses had come with their families to join in the celebration. Both of these patients I knew well and it is their stories that I want to share.
DL is a 10 year old who was admitted to Tenwek with acute pancreatitis. The exact cause was never clear- some thought it was “herb” ingestion. Home remedies from local plants are often used to treat illnesses in our region. Herbs are often toxic and it may be that DL’s pancreatitis was a result. Regardless, his pancreatitis was really bad and within a few days his abdomen was distended like a tight balloon to the point where he had difficulty breathing. Many liters of fluid were removed and analysis showed that it was pancreatic fluid. In a couple of days he re-accumulated and again the fluid was removed. This cycle continued on and on as a result of rupture of his main pancreatic duct. This made him quite ill. He couldn’t eat and he was in constant pain. Repeated attempts were made to use feeding tubes snaked beyond his stomach to provide nutrition, but even this resulted in vomiting. He was wasting away from malnutrition and we were forced to start nutrition through his IV. This is regularly done in the U.S., however, in our setting it has been difficult to safely and reliably use this form of nutrition for extended periods of time. But our team was incredible. The nurses worked tirelessly caring for this incredibly sick young man. Four surgeons from our team worked together, including our pediatric surgeon, the admitting general surgeon, and the two of us who work as critical care surgeons. I consulted with a hepatobiliary surgeon in the U.S., and a visiting gastroenterologist performed multiple procedures attempting to deal with the leaking duct. DL had all sorts of problems during his stay- the most alarming was a severe stomach bleed which resulted in such brisk bleeding that his heart briefly stopped requiring CPR. One day, 60 days after his admission and after I had returned from a short vacation, I came in to see him. He looked better but still wasn’t eating. We had tried many times to feed him, but his GI tract simply would not tolerate food. However, today something looked different. So, we fed him and this day, he kept food down. The next day he ate more. The day after that even more. Within 3 days we were able to stop his IV nutrition and within a few more days we were discharging him from the hospital.

DL along with his family.
The other patient who joined us at critical care day is PN. He is a patient who came to Tenwek with a life-threatening infection of his right thigh which required an amputation of his entire leg at his hip late one Friday night. This surgery is a highly morbid operation usually performed as an act of desperation to attempt to control infection. I took over his care as the surgeon on all on Saturday and we returned to the operating room to be certain that the infection was controlled. We discovered bowel contents pouring between the muscles separating the abdominal cavity from the thigh. So we explored his abdomen and found appendicitis which had perforated at its base on the large bowel requiring us to remove this segment of his intestinal tract. It was clear that this was the source of his original infection and what appeared to be a muscular infection of the thigh was in fact perforated appendicitis gone crazy. We found liters of foul-smelling pus around his right kidney and behind his liver. Over the next few days we made several trips to surgery to control the infection. The infection also spread to his right chest cavity which eventually required us to take him again to surgery to wash out his chest. We found extensive infection of his chest wall and it was clear the this was a no-win situation. Instead of proceeding with what would have been a radical debridement of his skin and soft tissue we decided that the situation was futile. The infection seemed to be beyond what we could treat. Chaplain staff visited with him. He re-affirmed his faith and was even baptized while he was in the ICU. We kept him on antibiotics but expected him to pass at anytime. Two weeks later, we were still rounding on him. Bewildered, I chose to change course and to step up our care. No longer were we simply doing “comfort measures.” A couple of our residents labored to be certain that he was getting adequate nutrition. Within a week PN was gaining weight and looking better. Ultimately I took him back to surgery for a thoracotomy to clean out the residual infection in his chest. A week after this, all of his drainage tubes were removed and he was sent home. PN maintained an incredible spirit throughout his entire stay. Our entire team noted his persistent smile even during the worst times. He shouldn’t have lived, but here he was now talking to us in a conference expressing his gratitude to God and the critical care team for seeing him through such a difficult situation.

PN and his family. We made him an honorary member of the Critical Care Team.
Watching these two families and seeing these patients now fully recovered and living their lives filled me with gratitude to the point were I was almost overcome with emotion. I was not alone. Our critical care nurses were proud. Residents who had cared for these patients came by to see them for themselves. The consistent comment was: “That’s amazing. Look how fat they are!” All of us knew that something special happened here, and for me it was a shot in the arm that I needed. Afterwards I started my lecture- the thing that I thought would be the point of all of this. But by the time I started the first slide, I knew that it wasn’t.
Our family has spent 4 of the last 5 years at Tenwek, and I must admit that for me the thrill is gone. The victories often feel few and far between. We try to rationalize away the pain and sorrow by discussing our failures and creating action plans to improve “the next time.” We pray for God to be at work, recognizing clearly that true change is beyond our human abilities. But while I was lost in this struggle, our nurses, through their cultural values of relationship and thanksgiving, brought to light moments where they have seen God working. I had failed to see this as clearly as I should have. But as the day wrapped up, I left grateful for the work being done at Tenwek and for the opportunity to be a part of it. Most of all, I was grateful for the outcomes of these patients and to see their lives restored.
My Grown Up Christmas List (2018)
‘Tis the season… for our grown-up Christmas list again! It’s hard to believe that this will be our 5th Christmas since moving to Kenya in June 2014. Our first Christmas, we did not have a Christmas wish list. We were still trying to get our minds around our new life… missing “home”… surrounded by an unfamiliar culture… one with so much need… wanting to serve our Kenyan community in sustainable and meaningful ways but not sure yet what that looked like. But since then, Christmas has become our favorite time of year to be in Kenya. It is the time of year when we are most able to connect our two “homes” as we connect the giving spirit of our U.S. home to the urgent needs around us in our Kenyan home. Our wishes have gotten bigger each year, largely because we continue to see God provide above and beyond our expectations. Each year God has used YOU as a means of His provision to our ministry here at Tenwek Hospital. Read on for a review of Christmases past and our BIG wish for Christmas present…
Christmas 2015: Compassionate care fund for needy patients, and orphan outreach needs (sustainable tea plantation, food, clothing, and education). This was the first year that we truly began to experience the joy of being the conduit of your blessings to those in need around us during Christmas giving. We still support the Surgical Compassionate Care fund through our personal ministry account when patient needs arise (www.wgm.org/missionary/many). The orphan outreach ministry has become more self-sustaining through farming efforts and local churches.

Christmas 2015 at Kinduiwo Children’s Home
Christmas 2016: Ultrasound machine. This machine is one of the most useful pieces of equipment that we have. It is literally almost in constant use. We use it for assistance diagnosing life threatening problems in the middle of the night, for guidance with invasive procedures, to evaluate cardiac function in our critically ill patients, as well as many other purposes. It also allows our residents to become highly skilled in performing and interpreting ultrasound. It is really an amazing tool.

Surgical residents using ultrasound to evaluate a neck mass
Christmas 2017: IV Pumps. Many of you came out big-time to support this project. We were able to purchase 30 IV pumps which have dramatically improved the quality of care in our critical care units and on the obstetrical ward. We can now safely give medications which require precise dosing. Particularly in our critical care units, we have been able to better care for our many patients with septic shock as well as provide IV nutrition that had previously been difficult to do.

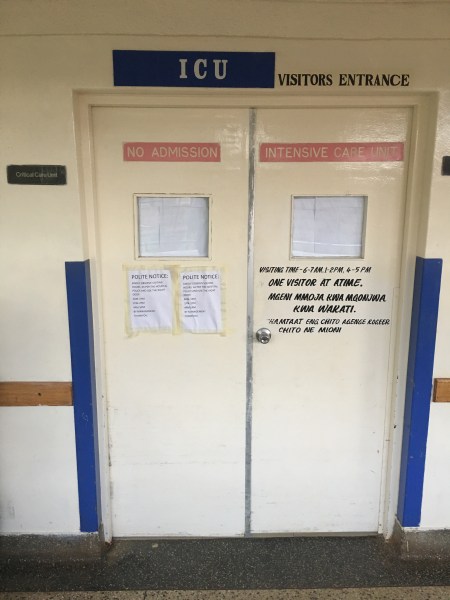
New IV pumps in use for an ICU patient
Christmas 2018: Resident Housing: Our calling to Tenwek Hospital was based on the need for well-trained surgeons in the developing world. Since we have been in Kenya, additional world-wide data has been published suggesting that roughly 5 billion people do not have access to safe, timely, affordable surgery and, not surprisingly, the people most affected by this fact are those in the developing areas such as sub-Saharan Africa. We are privileged to be a part of an amazing program that is training Christian surgeons in rural Africa. Currently we have residency programs in general surgery and orthopedic surgery. Graduates from our general surgery program are all working in East Africa, many of them in mission hospitals. The orthopedic program will graduate their first residents this year. However, we have been given a big opportunity to expand residency level training at Tenwek even further.
At the beginning of 2018, we accepted our first Cardiothoracic fellow into a three-year program. Tenwek is also moving forward with starting an OB/GYN residency program through the Pan-African Academy of Christian Surgeons with a tentative launch date as early as 2020. There is also enthusiasm for starting a neurosurgery residency program in the next few years. All of this is exciting and has the potential to make a big impact on health care in our part of the world. However, we have reached a major road block in our efforts. We have no housing for these trainees and will not be able to advance these programs until suitable housing is built.
Because of our rural setting, suitable housing close to the hospital is not available and therefore the hospital has to provide housing for those working at Tenwek. Currently we have housing to accommodate 23 residents. To begin any new program we need 16 more, but ultimately need about 35 more to allow us fill each of the proposed new programs as well as the existing ones. We have located property for a new apartment building which will house between 10 and 16 new resident trainees. Once this is built, we can then begin these new programs. The estimated budget for the building of this building including all the furnishings is $650,000.
This is a lot of money. However, if you think about it, this investment is a good one… one with long-lasting impact and eternal value! Our current buildings have allowed for the training and graduation of 12 surgeons with an additional 19 currently in the program who will graduate in the next 5 years. Additional housing will increase this number substantially as well as allow expansion of specialty training for many years to come. Are you willing to invest in equipping the next generation of physicians in East Africa and thus improve healthcare in an area with incredible need?
This CyberMonday, GivingTuesday, and Christmas season, consider spending money on sharing Christ’s love through medical training and discipleship! To give, visit Friends of Tenwek donation page here… and choose “Resident Housing Fund” on the drop-down menu.

Some residents and faculty with a current trainee apartment building in the background
Fire!
Posted on February 27, 2018 2 Comments
“There’s a FIRE!” These words interrupted our family movie night almost three weeks ago (February 9th) as our 11-year-old neighbor burst into our house, holding a lantern high, calling out the warning. Over the next several hours, a fire destroyed one of the buildings of Tenwek Hospital as Heath worked to evacuate patients, and Angela held vigil with several missionary kids ready to evacuate the compound if needed.
After our neighbor’s warning, we quickly stepped outside onto our porch. The first thing we noticed was the sound of screaming and wailing. Living so close to the hospital, it is not unusual to hear wails of mourning when someone dies. But the wails were much louder than a typical mourning of death. Also immediately noticeable was the thick dark smoke in the sky above the hospital, which sits about 100 yards up the hill from our house. Heath left quickly to go check out the situation.
Fire in rural Kenya is a powerful and deadly force. Everyone living here knows it to be so. History has shown fire-fighting capabilities to be unreliable at best, and built-in containment and extinguishing methods are absent. No automatic sprinklers were present to come on. No fire-safe doors were present to close. No fire alarms sounded…only the screams and wails mentioned earlier, which grew louder and louder over the next few hours as villages even miles away saw the increasing flames and joined in expressing their fear and grief. The first fire truck came from the next county, about 2 hours away. When the truck arrived, the water hoses attached to rain tanks in the truck didn’t stand a chance against the inferno.
So when Heath ran up to the hospital, he had no false sense of peace that help was on the way. The building on fire was the first building inside the staff gate. It housed the kitchen, restaurant, several offices (research, statistics, visiting staff, and social work) on the top-level; and laundry, sterilization, and a patient ward (Wound Ward) on the bottom level. Heath saw that the patients from the Wound Ward were almost all evacuated. By this point, the flames were massive. Heath found one of the other surgeons, and they tried to keep people away from the fumes and fire. Attention was quickly turned toward evacuating patients closest to the fire. The orthopedic ward was in an immediately adjacent building, so Heath made his way there to find that the power was out and patients were screaming for help. Although there was no fire in this building, huge flames were easily seen from the windows, and the heat of the flames could be felt by the patients who were stuck in their beds due to their orthopedic injuries. After getting some help, these patients were moved out on stretchers or dragged on mosquitos nets to an area further away from the fire.
While the fire continued to grow, Heath joined other physicians and staff who were starting to evacuate the intensive care units. Knowing these patients well, Heath stayed with these critically ill patients who had been moved to the maternity ward and the recovery room. By the grace of God, there were no patients on ventilators. Efforts were coordinated with a visiting team of pediatric critical care nurses and physicians to get our sickest children under their watchful eye in our recovery room area. This freed Heath up to more closely monitor the intensive care patients who were moved to the maternity ward. He recruited a couple of visiting medical students to help him with these patients. Because there was no advanced monitoring, patients were closely monitored by sitting at their bedside and monitoring their pulses and respirations. Thankfully, all patients did well.
Meanwhile, other physicians and nursing staff evacuated the less critically ill patients to our new eye building. Patients were pushed up hill along a rough dirt and gravel road to reach the eye building which was temporarily converted to a patient ward. Many patients who could walk simply fled the hospital by jumping over fences and making their ways through fields and small farms to get far from the flames. One young patient who was in the hospital getting care for severe burns panicked so much at the thought of being burned again that she ran 2 miles to the nearest small town.
In the eye ward, trouble arose when oxygen began running out. Fortunately, by this time the fire had largely burned itself out, and it appeared that it would not spread to the rest of the hospital. The patients requiring oxygen were quickly transported back to the main hospital wards, which was a dicey event due to a lack of portable oxygen tanks. Again, despite a few moments of desperation, all patients were successfully transferred back. Next, the critically ill patients were transferred back to the intensive care units.
During this entire event, our visiting pediatric cardiac team was operating on one of the most challenging cases of their entire visit. Due to difficulties getting the child off the cardiac bypass machine, the surgery went into the wee hours of the morning. Despite being in a hospital on fire, they continued to operate, and ultimately the child was weaned from bypass and brought to the recovery room well after the last flames had gone out.
While Heath was busy moving patients, Angela hosted a “safe-house” where several families and missionary kids (whose parents were up helping with the fire) hung out waiting to possibly evacuate the compound. Everyone had passports and cash in the car, ready to drive away if the fire began to spread. From our perspective down the hill, we could see only a wall of giant flames, with no knowledge of how much of the hospital was burning. Our sky was filled with thick smoke, the loud sounds of popping glass and tiles, and the African-styled wailing. Cell service was down, so communication was very limited. Rees and Mary Taylor stayed calm despite their fears, and used what they had to help calm the younger children (songs, stuffed animals, prayer, and encouraging words).
We praise God that the fire was contained to one building, and specifically, that the Boiler and Generator buildings were spared. We remain amazed at His protection over patients, staff, and volunteers…NO one was injured! We are grateful for the stone walls and cement floors that likely helped to prevent further spread. Wood fencing, edging and roofing were torn down manually during the fire to also help prevent spread. We are also grateful to all of the staff and community members who bravely fought the fire with buckets of water and small fire extinguishers.
Pastoral staff and a counseling team were on site the next morning, meeting with staff, patients, and community members for post-crisis intervention. Many staff and families have gathered to share their stories with each other and have participated in counseling provided. We have had an incredible outpouring of support from the community, county and national governments, and international partners.

Hope from the ashes…A beautiful promise over the destroyed building!
For the current time, Wound Ward has been relocated to the former Eye Ward. Kitchen services have been temporarily shifted to the Tenwek Hospital College of Health Sciences Kitchen. The lower level services of Sterilization, Laundry, and Tailoring were restored within the first week. The offices on the main floor of the building are being relocated to other areas. Therefore, the hospital is back in service!
Tenwek Hospital Administration is now evaluating the best ways to restore services long-term and fulfill the ministry of Tenwek Hospital. Even this week, an engineering and architectural partner will arrive to give input.
THANK YOU to those who stepped in so quickly to contribute financially toward the rebuilding process. Many of you give faithfully already to our ministry here, yet you have responded readily in our time of need. “Thank you” seems so insufficient!
If you still wish to give toward the recovery effort, please give through this link: Tenwek Hospital: Fire Recovery. We hope to have ability to not only rebuild, but to also install some appropriate fire safety and prevention measures throughout the rest of our hospital.
Full healing will take time. Please pray for the patients who came to a place of safety and healing, and instead experienced a terrifying event… for our Administrative staff as they seek wisdom in rebuilding… for our community to continue to pull together in support of one another… and for God to be glorified even in this tragedy. Please continue to pray for our family as we seek to live out the motto of Tenwek Hospital: “We treat ~ Jesus heals.”
Our worship team singing ”Jesus is the Rock” in Swahili the day after the fire in our church which sits a mere 20 feet from the destroyed building. Thank you Jesus for being our Rock! (You might recognize a singer and ukulele player here!)
My Grown Up Christmas List
Posted on November 30, 2017 2 Comments
(3rd Annual)
Well friends, here it is…My 3rd annual Grown Up Christmas List! When I began this wish list three years ago, our second Christmas in Kenya, I was struggling to come to terms with the reality of deep needs all around me in my new life…needs that overnight had gone from being statistics and maps, to patients and neighbors and friends. I desperately desired to give meaningful ways for my circle in the US to engage with our needs here in Kenya. You have stepped up in amazing ways to help meet to our ministry needs, and we have been so blessed to be the conduit of your blessings to our community!
Last year, through your generous year-end gifts we were able to help purchase a much-needed ultrasound machine for the Surgery Department! It has been put to great use for improved pre-operative evaluation, post-operative patient care, ultrasound-guided procedures, and resident education. There were also gifts given toward our local orphan ministry, help in spreading the word about our need for a teacher, and ultimately gifts toward supporting Grace (our teacher) as well.

Heath using the new ultrasound machine to evaluate a post-operative cardiac patient.
This year, our wish is to raise enough funds to buy IV pumps for our Intensive Care Units and Maternity (L&D). This may not sound like a very “exciting” need, but caring for patients who require certain critical medications without an IV pump is incredibly difficult! It means that we must count and time the drips carefully and readjust the tubing manually to get the drip-count just right for the accurate dose. Not only is this tedious and difficult, but it is risky for patients as they can easily be given too much or too little medication.
To further express the impact that this has on patient care, Heath will share about one of his recent patients…
My first few calls after we returned to Tenwek were busy ones. Between civil unrest due to elections and a nation-wide nursing strike we were slammed with surgical emergencies. Late one afternoon, a woman came to casualty complaining of abdominal pain after spending several days at another hospital. It was clear that she had some sort of catastrophic problem in her abdomen which would require surgery. Her blood pressure was low which required the administration of many liters of IV fluid to correct, and after we had done so, we took her to surgery. While there we found that she had a gangrenous segment of intestine which had perforated- clearly this was a problem that had gone on for days. During the procedure her blood pressure continued to drop forcing us to start her on medication to raise her blood pressure, and we performed an abbreviated operation so that we could get her out of the OR and to the ICU. After transporting her to the ICU, she continued to need a couple of medications similar to adrenaline (we refer to these drugs as vasopressors) to maintain her blood pressure. These medications must be carefully titrated in relatively small amounts to prevent complications. In the U.S., we use electronic IV pumps to control the rate of delivery of these medicines. At Tenwek, we have a very limited number of IV pumps and there were none available this night. So, we mixed up the medicines in large bottles of saline and began the tedious task of counting the number of drips of fluid over a minute so that we could determine the dose of medicine she received and then make adjustments to the rate accordingly. We spent a couple of hours at her bedside watching her blood pressure and counting and adjusting drips. Despite our efforts, our patient died a few hours later- her infection was simply too advanced, and she received treatment too late. However, our experience that night brought to light one of the biggest issues we (and especially our nurses) wrestle with in our intensive care units- lack of IV pumps. It is clear that we will have a hard time improving the quality of care of our most critically ill and injured patients without suitable IV pumps.
……..
One IV pump costs $1500. We would like to purchase 25 pumps for use in our ICU and Maternity areas at Tenwek Hospital. Can your family, business, or church group come together and purchase an IV pump? It would make a life-changing Christmas gift for a patient in need!
To give toward this project, click HERE. This goes directly into our ministry account. All gifts that we receive in December will go toward the IV pump project. Feel free to contact us if you have additional questions. We will update you after Christmas with the outcome!

Our current IV set-up. Count… the… drip… drip… drip…
As the song lyrics say, “But Heaven only knows, That packages and bows, Can never heal a heartached human soul.” We know that our material gifts will always fall short of meeting the deepest need of the soul. We pray that as we attend the physical needs of the patients under our care to the best of our ability, with kindness and compassion, that we can show the love of Christ, pointing to the giver of all gifts and the healer of our souls.
We hope that your Christmas season is filled with reminders of God’s love and His gift of a savior in Jesus. Thank you for helping us share that gift in Kenya.
Trauma and Critical Care Training: What was I thinking?
Posted on October 2, 2017 2 Comments
At some point in 2004, I walked out of the Univeristy of New Mexico Hospital with a smile on my face. I had just completed my last day on the trauma service. No longer would I be up in the middle of the night taking care of labor-intensive injured patients. No longer would I sit for hours in the ICU taking care of the sickest of sick patients while others operated on the “interesting cases.” My career path was taking me towards the aspect of surgery that I loved the most- operating, operating, operating. I was happy to be in the OR all day while critical care specialists helped take care of the sicker patients whose care I was involved in.
I spent the first decade of my career as a busy, private practice surgeon which meant I spent a lot of time in the operating room. I loved it. But as our family transitioned to Kenya it became very apparent that good outcomes in complex surgical patients at Tenwek were hard earned. Yes, a technically perfect operation is imperative, however, a good outcome depends on much more than just a good operation. Technically difficult operations could be completed, however, patients who became sick after these procedures or who were admitted to the ICU after life threatening trauma often times died when they shouldn’t have. Was it my care? Was it the residents’ lack of knowledge of critical care medicine? Was it our monitoring capabilities? Was it nursing? Was it specific problems in our rural Kenyan population? The answer to all of these questions was yes. And there are many more problems. The bottom line is that it is largely a systems issue. We as physicians like to tackle specific diseases and problems, but we often times neglect the development of a system of care that can be applied to a broad range of patients. It became clear to me that we can teach our residents how to be expert operators- even at advanced techniques such as laparoscopy that are rare in rural Africa. However, until we develop a better system for caring for the critically ill, outcomes in our sickest patients are not likely to change.
As our first term in Kenya was coming to an end in June of 2016, we began to think about how we would spend our time in the U.S. Angela and I had decided that we wanted the girls back in school for a complete school year. Angela wanted to mainly focus on helping the girls transition back to the U.S., and I hoped to be able to work. But as I thought about working, I felt like my time would be best spent by trying to learn things that I could take back to Kenya. We discussed the possibility of me doing a fellowship in surgical critical care and ultimately decided to ask around to see if there were any available fellowships spots. Fellowships are additional training programs that physicians can do once they have completed a residency. To be a cardiologist, one does a fellowship after a medicine residency. To be a heart surgeon, surgeons will do a 2 or 3 year fellowship after their general surgery residency. Surgeons can do a year of specialized training in surgical critical care which prepares one to care for the sickest of sick surgery patients. In practice, most surgical critical care specialists are also trauma surgeons due to the fact that traumatized patients often make up a large percentage of patients in a surgical ICU. In the current era, the evolving specialty of acute care surgery has emerged, which encompasses surgical critical care, emergency general surgery, and trauma surgery (which makes up a huge chunk of what we do at Tenwek). Most practitioners of this specialty in teaching facilities are board certified in surgical critical care. And so, my hope was to find a fellowship which would allow me to do this.
After sending out multiple inquiries, we were delighted to hear that the program at the Univerisity of Tennessee in Knoxville was willing to allow me to join them for a year as one of their surgical critical care fellows. I couldn’t be more grateful to the trauma and critical care faculty at UT who helped create a spot for me. They allowed me the freedom to spend time learning skills would be beneficial to the work at Tenwek. I was even able to spend a month at Parkwest Hospital (the hospital were I worked prior to going overseas) working with the cardiac anasthesiologists learning how to take care of cardiac surgery patients. However, the year of training had its struggles. I felt all of my 43 years of age during the busy call nights. Recovery after these busy call nights took an extra day or two more than it used to. Time with our family was more limited than we had hoped after being away for a couple of years. However, it was a privilege to have the opportunity to sink my teeth into learning the nuances of trauma and critical care surgery.
Now as we transition back to Tenwek I am looking forward to putting new knowledge to work. Like many other areas of medicine, modern critical care capabilities are lagging in the developing world. In Kenya, there are nicely developed critical care units in some of the larger hospitals in Nairobi, however, distance, money, and transportation issues limit access to these facilities for a large percentage of the population. Fortunately, the need for surgical ICU development in low and middle-income countries is increasingly recognized. A nice article by Drs. MacLeod, Kirton, and Maerz was published in 2016 highlighting the incredible need for critical care development as well as possibilities for a way forward in development. Here is the link to this article for all of you as nerdy as me: Surgical Intensivist and global critical care: is there a role? The authors point out staggering statistics such as the fact that 90% of deaths due to trauma world-wide occur in low and middle-income countries. Each year, 8 to 10 million children under the age of 5 die, however, 90% of these deaths occur in the 42 poorest countries. Many of these deaths could be prevented by access to critical care services. Although ICU’s in the west are often thought of has being high-tech, expensive, sophisticated units, the authors correctly point out that major improvements in patient outcomes can be achieved by implementing basic tenets of critical care. It is my hope to continue to make improvements in the way we deliver surgical critical care in our relatively rural setting at Tenwek, but more importantly, to educate our residents so that when they leave our program they are capable of ministering to the sickest of sick.
Wishes coming true!
Posted on May 17, 2017 Leave a Comment
God has answered SO many prayers of our hearts during our time in the U.S. this year! We want to share some amazing follow up on my wishes from “My Grown Up Christmas List”…
A TEACHER!… We have a teacher preparing to join us in Kenya! Grace Williams graduated from Johnson University in Knoxville in 2016 in Early Education. She heard of our need for a teacher through our video shared by her Education Department. Realizing that she had the skill set, desire, and ability to help meet this need, God worked through her heart and circumstances to bring her to a willingness to serve with our team. She will be teaching 3rd and 4th grade missionary kids and working with children’s ministries at our Kenyan church. I know she will be a huge blessing to our family and the rest of our team! Please pray for Grace as she takes this step in faith to live and work in Kenya. Grace will be raising her own support for this year. If you would like to contribute to her financial support, click here.

An ULTRASOUND machine!… Thanks to the generous donations of several couples, a matching gift from Friends of Tenwek, and a discount given by Sonosite, we were able to purchase a new Ultrasound machine for Tenwek for use in the surgery department. This is a new machine with fantastic imaging capabilities that will add immensely to our patient services and resident education. The machine has arrived and is already in use at Tenwek!

Surgery team with new US

Two residents using the US for patient exam
EDUCATION for an orphan… This is always an ongoing need! As I have shared before, education is one of the BEST investments in helping vulnerable children rise above poverty and other risks. We have had many friends and church groups invest money toward our Tenwek orphan scholarship fund. Thank you! This week, Mary Taylor’s grade at school held a “Coins for Kenya” walk to raise money for a child’s school fees. They learned about the difficulties that many children face in going to school and brought in their coins to help pay for a year of schooling for a child in Kenya. I pray that God will move in these young hearts to know that they are a part of His story, and that even they can be used to show His love to others around the world! If you feel led to help sponsor a child’s schooling, click here.

Mary Taylor and classmates collecting “Coins for Kenya” from the 3rd grade

High school orphans getting help with school supplies to begin second term earlier this month
My Grown up Christmas List
Posted on November 30, 2016 1 Comment
(2nd annual)
Tis the season! No better day than “Giving Tuesday” to roll out my 2nd annual Grown up Christmas List! Even though this year we will have the joy of celebrating Christmas in America, our hearts and minds are still with our Kenyan friends and neighbors. Throughout the past few years, our vision has grown bigger, our passion deeper, and our excitement greater about what God is doing in East Africa through Tenwek Hospital, our PAACS graduates, and our local Kenyan church. Although it has been humbling and challenging to live and work in an area of the world with such great need, it has also been rewarding beyond measure. I know that our blog has been silent since our return to the US this past summer. We have found it difficult to express in words the ups and downs of living between two “homes.” Returning to the US with fresh eyes has been interesting! Maybe we will share more in a future post about the good, the bad, and the ugly of this fresh perspective. But one surprising outcome of our experience so far in serving as “missionaries” is the amazing way that God has allowed us to connect so many people within our circle (and even beyond) to His work in the world. Ironically, even though we have “less” by the world’s standards now, we have been able to GIVE even MORE…by being conduits of your blessings which have been given so generously. We have been continually amazed at how God has used YOU (our community in America) to bless our community in Kenya! So in this season of giving, we wanted to again highlight some needs near to our hearts. If you are hoping to make a real difference with your dollars this Christmas season, instead of more online shopping for more “stuff”…consider one of our wish-list items below!
1. EDUCATION for an orphan..
Schooling in Kenya is not free…One year of tuition and required school fees (books, uniforms, food, etc.) costs about $500 per child. Orphans are especially at risk for not progressing through school due to lack of financial support among other factors. Access to education for orphans and vulnerable children has been directly linked to improved health, wellbeing, and long-term outcomes. Our local children’s homes care for about 350 orphans who rely on donations to provide this critical opportunity for education. Could you give a child the gift of knowledge and opportunity this year? If you can’t give $500, any amount does help! If this need speaks deeply to you and you have interest in a commitment each year to sponsor a child’s schooling, please contact me for more information.
Donate directly at Tenwek Orphan Scholarship Fund

Mary Taylor playing with a friend at a local orphan home
2. An ULTRASOUND machine for surgical use…
Ultrasound is a vital tool for patient care at Tenwek Hospital. Our radiology department does about 50 patient scans per day, leaving little availability for ultrasound use in surgery, in evaluating trauma and critical care patients, or in teaching residents these important skills. We are in dire need of an additional ultrasound machine devoted to these purposes. We are raising funds to purchase a Sonosite M-turbo portable machine. Sonosite has offered a generous discount, and Friends of Tenwek organization is contributing 50% of the needed funds! Could you help us in raising the additional 50% needed to acquire this important tool for improving patient care and training?
Donate directly to this need at Surgery Dept. US Project

Family medicine resident, Elijah, evaluating a pediatric patient for pleural effusion
3. A TEACHER!
OK, so this isn’t something that money can buy at all, but it is my biggest wish! Our Tenwek community is in need of two teachers committed to helping with educating our missionary kids. This important job impacts our ministry in such a big way! If you or someone you know is a teacher licensed for elementary or middle school with a heart for missions and a willingness to consider serving with us in Kenya, please contact us! Help spread the word!

Tenwek MKs playing on a beautiful Kenyan afternoon
Thank you for considering supporting our Kenyan community and our work at Tenwek Hospital. We look forward to returning to Kenya in 2017. Thanks to our amazing partners, we have 95% of our needed monthly funds for our return already committed! Are you interested in joining our support team? If so, contact us to learn more, or donate directly toward our ministry . We are in currently Knoxville, where Heath is doing additional training in critical care at UT Hospital, and Angela is working to juggle our family’s transition. If you would like to connect, please contact us!

Our family’s last hike up our local “mountain” before our return to the US this summer
All of this is for your benefit. And as God’s grace reaches more and more people, there will be great thanksgiving, and God will receive more and more glory.” ~2 Corinthians 4:15 NLT






